Total Hip Replacement Surgery (Arthroplasty)
Replacing the damaged hip joint to relieve pain and improve movement in patients with advanced arthritis
Total hip replacement surgery is a common and effective procedure used to treat advanced hip arthritis and other degenerative joint conditions when non-surgical treatments are no longer providing adequate relief. The surgery involves replacing the damaged surfaces of the hip joint with artificial components, with the goal of reducing pain and improving function.
The hip joint plays a central role in mobility and balance, so when it becomes painful or stiff, it can significantly affect your daily life. Total hip replacement may help restore movement and improve your overall quality of life.
Dr Scott Tulloch uses modern surgical techniques and pre-operative planning tools to ensure each procedure is carefully tailored to the individual. In the following sections, you’ll find clear information about what to expect before, during, and after surgery, as well as the specific approaches and technologies used in your care.
- Signs You Might Need A Hip Replacement
- Factors That Make You A Good Candidate For A Hip Replacement
- When A Hip Replacement Might Not Be Right For You
- Total Hip Replacement Surgical Techniques
- Personalising Your Hip Replacement Procedure With Technology
- The Hip Replacement Prosthetic Implants: Design, Structure, And Durability
- Understanding The Risks Of Hip Replacement Surgery
- Benefits Of Hip Replacement Surgery
- Pain Management After Total Hip Replacement Surgery
- Recovery Following Total Hip Replacement Surgery
- Post-operative Precautions Following Total Hip Replacement Surgery
- Long-term Care For Your New Hip: Tips & Guidance
- Self-funding Your Total Hip Replacement: A Guide For Patients Without Private Health Insurance

Signs You Might Need A Hip Replacement
Deciding on hip replacement surgery is a significant step, usually considered when severe hip pain and restricted movement profoundly affect your quality of life.
Understanding the conditions that may lead to surgery is essential, as it helps in recognising the symptoms and diagnoses that might indicate the need for a hip replacement:
- Osteoarthritis: This is often the most common reason for hip replacement. Osteoarthritis involves the breakdown of cartilage in the hip joint, resulting in pain, stiffness, and reduced mobility.
- Rheumatoid Arthritis: As an autoimmune disorder, rheumatoid arthritis causes chronic joint inflammation. This can lead to significant damage and pain in the hip, making replacement surgery a possible solution.
- Avascular Necrosis: When blood flow to the hip bone is reduced, avascular necrosis may occur, leading to bone deterioration and severe pain, often requiring hip replacement.
- Hip Fractures: Especially in older adults, hip fractures may necessitate a hip replacement to restore joint function and relieve pain.
- Congenital Hip Dysplasia: If you were born with abnormalities in your hip joints, you may experience pain and instability. Hip replacement surgery may become necessary if other treatments are unsuccessful.
- Post-Traumatic Arthritis: Arthritis that develops after a significant hip injury or trauma can lead to joint damage, making hip replacement a viable option if other treatments have not provided relief.
- Other Conditions: Various other issues, such as certain bone tumours, infections in the hip joint, and systemic diseases affecting the joints, may also necessitate a hip replacement.
t’s important to understand that the decision to undergo hip replacement surgery is a personal one and varies from patient to patient. The choice is based on a thorough evaluation of your specific situation and how much your daily life and mobility are affected.
During your consultation, Dr. Tulloch will conduct a comprehensive assessment of your condition. This includes a detailed discussion about your symptoms, an examination of your hip, and a review of your overall health and lifestyle. Together, with Dr. Tulloch, you will explore whether hip replacement is the most effective way to improve your mobility, alleviate pain, and enhance your quality of life.
Factors That Make You A Good Candidate For A Hip Replacement
Deciding to undergo hip replacement surgery is a significant decision, influenced by various factors related to your health and lifestyle. Dr. Scott Tulloch takes a personalised approach to determine whether you are a suitable candidate for this procedure. Here are the key factors considered during your evaluation:

- Chronic Pain: Persistent hip pain that significantly affects your daily activities and does not respond to non-surgical treatments is a primary indicator. This pain may interfere with simple tasks such as walking, climbing stairs, or even resting.
- Limited Mobility: A reduced range of motion and stiffness that limits your ability to perform routine activities is another crucial factor. If you find it difficult to bend, rotate, or move your hip normally, hip replacement might be necessary.
- Quality of Life: If your hip condition severely impacts your quality of life, causing you to limit your social activities, hobbies, or work, you may be a candidate for hip replacement surgery. The goal is to restore your ability to engage in these activities without pain.
- Failed Conservative Treatments: Candidates for hip replacement are typically those who have tried and failed conservative treatments, such as medications, physiotherapy, or lifestyle modifications. If these treatments have not provided sufficient relief, surgery may be the next step.
- General Health: Your overall health plays a significant role in determining your suitability for surgery. Dr. Tulloch will assess your medical history, including any chronic conditions such as diabetes or heart disease, to ensure you can safely undergo the procedure.
- Weight: Maintaining a healthy weight is important for a successful hip replacement. Excess weight can put additional stress on the new hip joint, affecting its longevity and your recovery process.
- Bone Health: Strong, healthy bones are essential for the success of a hip replacement. Conditions like osteoporosis can affect the stability and integration of the hip implant.
- Age Considerations: While hip replacements are more common in older adults, younger individuals with severe hip damage may also be considered. The decision is based on the extent of hip degeneration and the impact on your life rather than age alone.
- Activity Level: Your desired activity level after surgery is also taken into account. Dr Tulloch will discuss your lifestyle goals and how a hip replacement can help you achieve them, whether you aim to return to sports or simply enjoy pain-free mobility.
- Mental and Emotional Health: Being mentally and emotionally prepared for surgery and the recovery process is crucial. Dr Tulloch ensures that you understand the procedure, the rehabilitation involved, and the realistic outcomes to help maintain a positive mindset and adherence to post-operative care.
While total hip replacement is commonly performed in older adults, younger patients with significant hip damage may also be suitable candidates. Dr. Tulloch assesses each case individually, focusing on the extent of joint degeneration and how it affects your daily life, rather than age alone.
Your activity goals after surgery are also an important part of the discussion, whether you’re hoping to return to recreational activities or simply move without pain. Dr. Tulloch will take the time to understand your lifestyle and guide you through what a hip replacement may realistically offer. Being prepared both mentally and physically for surgery and recovery can play an important role in achieving a smoother outcome.
When A Hip Replacement Might Not Be Right For You
While hip replacement surgery can provide substantial relief and restore mobility for many individuals, it is not the right choice for everyone. Several health conditions and factors may contraindicate the procedure, making it essential to thoroughly evaluate your overall health and specific circumstances before deciding on surgery.
Common Conditions That May Prevent Immediate Hip Replacement Surgery
- Active Infections: If you have an active infection anywhere in your body, particularly around the hip joint, surgery is generally postponed. Infections pose a high risk of spreading and can complicate the healing process, potentially leading to severe complications.
- Severe Medical Conditions: Individuals with uncontrolled chronic health issues such as advanced heart disease, severe diabetes, or serious respiratory conditions may not be suitable candidates for hip replacement. These conditions elevate the risks associated with anaesthesia and surgery and may impede recovery.
- Weakened Immune System: A compromised immune system, whether due to conditions like HIV/AIDS or the use of immunosuppressant medications, can increase the risk of post-operative infections and slow down the healing process.
- Severe Osteoporosis: Significant bone density loss, such as in severe osteoporosis, can undermine the stability and fixation of the hip implant. In these cases, the bones may be too fragile to support the new joint effectively.
- Complex Joint Deformities: Severe deformities or significant anatomical abnormalities of the hip joint may complicate the surgery and affect the overall outcome. Dr. Tulloch will carefully assess the severity of these conditions to determine whether surgery is the best option or if alternative treatments are more appropriate.
- Blood Clotting Disorders: Patients with bleeding or clotting disorders, such as haemophilia, may face increased risks during surgery. Comprehensive management and assessment by a haematologist are often necessary to evaluate the safety and feasibility of proceeding with the procedure.
- Excessive Body Weight: Obesity can put additional stress on the hip joint, both during surgery and throughout the recovery period. Being significantly overweight may also increase the likelihood of surgical complications and can impact the longevity of the hip implant.
- Severe Neurological Conditions: Neurological disorders, such as Parkinson’s disease or severe neuropathy, can impair your ability to follow rehabilitation protocols after surgery, which is crucial for a successful recovery.
- Mental and Emotional Health: Psychological readiness is vital for the success of hip replacement surgery. Severe depression, anxiety, or cognitive impairments can interfere with your ability to comply with post-operative care instructions and engage effectively in rehabilitation. A stable mental and emotional state is crucial for a smooth recovery.
- History of Non-Compliance: A history of not adhering to medical advice or rehabilitation protocols may be a contraindication for hip replacement surgery. Compliance with post-operative care is critical for achieving the best possible outcomes.
- Substance Abuse Issues: Ongoing issues with drug or alcohol abuse can interfere with both the surgical procedure and the recovery process. It’s important to address and manage these issues before considering hip replacement surgery.
Dr. Tulloch will carefully evaluate these and other factors during your consultation to ensure that hip replacement surgery is the safest and most effective option for you. The goal is to maximise the benefits of the surgery while minimising any potential risks.
Total Hip Replacement Surgical Techniques
Total hip replacement surgery involves the precise removal of damaged or diseased portions of the hip joint and replacing them with prosthetic components. The choice of surgical technique is crucial and depends on several factors, including your anatomy, the extent of the damage, and your surgeon’s expertise.
Here is an overview of the primary surgical techniques used in hip replacement:
The direct anterior approach (Anterior Minimally Invasive Surgery (AMIS)) is a minimally invasive technique that involves an incision made at the front of the hip. This method allows your surgeon to work between muscles and tissues without cutting through them, which can lead to a faster recovery, less post-operative pain, and a shorter hospital stay. This approach is particularly suitable for patients who prioritise a quick return to their normal activities. It does, however, require a high level of specialised training and extensive experience, both of which Dr Tulloch has meticulously developed through years of dedicated practice and advanced education.

The posterior approach is one of the most widely used techniques in hip replacement surgery, primarily because it provides excellent visibility and access to the hip joint. This approach has become popular due to its versatility and the familiarity surgeons have with the technique. It’s important to note however, that being widely used doesn’t always mean it’s the best option for every patient. The posterior approach involves cutting through some muscles at the back of the hip, which are then carefully reattached during the procedure. With proper rehabilitation, patients can achieve a successful recovery of hip function.
Dr. Tulloch may choose this technique in specific circumstances where the benefits of enhanced visibility of the hip joint outweigh other considerations, ensuring the best possible outcome for the patient.
The SuperPATH approach (short for superior percutaneously assisted total hip replacement) is a more recent variation of the posterior technique. It is designed to minimise tissue disruption by working between muscles rather than cutting through them. This can make the approach less invasive while still allowing access to the hip joint.
Unlike the traditional posterior method, the SuperPATH technique typically avoids detaching major muscles or tendons. This muscle-sparing approach may support faster recovery, reduced pain, and a lower risk of hip dislocation in some patients. It’s important to remember, however, that no single approach is best for everyone.
Dr Tulloch may recommend the SuperPATH approach for patients where tissue preservation is a priority and the anatomy is suitable, always aiming to tailor the procedure to each individual’s needs and goals.
The lateral approach involves an incision made on the side of the hip, offering good access to the hip joint while balancing stability with the preservation of some muscle function. This approach is often selected for patients with specific anatomical considerations or those who may be at a higher risk of hip dislocation. However, it is important to note that the lateral approach involves detaching and splitting the hip abductor muscles (gluteus medius and minimus), which can sometimes result in a permanent limp due to the muscles’ inability to fully stabilise the hip after surgery. Bone growths, or ossifications, may also develop in the damaged gluteal muscles.
Although recovery times may be slightly longer compared to the anterior approach, the lateral approach remains a reliable option for a wide range of patients, particularly when other techniques may not be suitable.
Dr. Tulloch does not typically use this approach for his patients, preferring other methods that better align with his goal of optimising patient outcomes and minimising post-operative complications.
The anterolateral approach to hip replacement involves accessing the joint from the front and side of the hip. This technique aims to preserve muscle while still providing good visual access to the hip joint, making it a viable option for selected patients.
The approach typically works between muscle groups rather than cutting through them, particularly the gluteus medius and minimus. By preserving these important muscles, it may help maintain hip strength and support post-operative stability.
While the anterolateral approach avoids detachment of key tendons, it can place traction on surrounding muscles and nerves. For this reason, it is less commonly used in Australia but may be considered in specific cases where the benefits outweigh these risks.
Personalising Your Hip Replacement Procedure With Technology
Hip replacement surgery has seen remarkable advancements, significantly enhancing both its safety and effectiveness. Modern procedures now utilise advanced materials such as metals, ceramics, and highly cross-linked polyethylene, combined with cutting-edge surgical techniques. The introduction of robotic-assisted procedures, patient-specific technologies, and custom 3D-printed implants tailored to match each patient’s unique anatomy has further improved the potential to reduce recovery times and enhance functional outcomes for patients undergoing the procedure.
Dr. Tulloch is at the forefront of these innovations, employing minimally invasive surgical techniques that prioritise patient recovery and long-term success. He particularly favours the anterior approach, known for its smaller incisions and reduced impact on surrounding tissues, which can result in quicker recovery and less post-operative pain. However, Dr Tulloch always adopts a personalised approach, carefully evaluating how each technique aligns with the specific anatomies and lifestyle needs of his patients. This ensures that every surgery is as effective and tailored as possible.
Some of the technologies Dr Tulloch may utilise in a total hip replacement surgical procedures include:
PATIENT-SPECIFIC INSTRUMENTATION (PSI) MyHip
Patient-specific hip replacement surgery (PSI), also known as a customised total hip replacement procedure, involves using advanced tools, to create a highly tailored surgical plan based on your unique anatomy. This approach utilises 3D imaging and specialised software to meticulously plan the placement and alignment of the hip implant components. By creating a detailed, virtual model of your hip, Dr. Tulloch can simulate the surgery ahead of time, aiming to match the size and orientation of the implant closely to your natural hip joint. This precise planning is designed to improve functionality, comfort, and overall surgical outcomes by reducing the likelihood of alignment issues during your procedure and ensuring that your new hip fits as naturally as possible.
How the patient-specific total hip replacement procedure works:
- Pre-Operative Scanning: The process begins with a pre-operative CT scan of your hip joint (at least 6 weeks before surgery). This scan provides detailed images that are used to create a virtual 3D model of your hip anatomy.
- 3D Preoperative Planning: Using specialised software, Dr Tulloch can plan the placement and alignment of the hip implant components based on your specific anatomy. The aim of this is to closely match the size and orientation of the implant to your natural hip joint, which may help improve functionality and comfort.
- Customised Surgical Guides: Based on the 3D model, customised surgical guides are created using 3D printing technology. These guides assist Dr. Tulloch during your procedure by helping to ensure that the implant is placed with a high degree of accuracy. The customisation provided by these guides facilitates the precise placement of your hip implant, ensuring it fits securely and is unaffected by any movements during surgery. This adaptability allows the technology to be finely tuned to your unique needs, potentially improving the accuracy of implant sizing and positioning.
ROBOTIC-ASSISTED SURGERY
Robotic-assisted surgery represents a significant advancement in the field of hip replacements, offering a highly precise approach to the procedure. This technology allows for the creation of a detailed 3D model of the patient’s hip, enabling Dr. Tulloch to carefully plan the surgery and position the implant with a high degree of accuracy. By enhancing the precision of implant placement, this method aims to improve the alignment of the hip components, which may contribute to favourable long-term outcomes and help reduce the risk of complications.
This advanced technique involves:
- Enhanced Precision: Robotic systems assist in the accurate placement of implants, improving the alignment and fit of the artificial components.
- Customised Planning: Pre-operative planning with 3D imaging allows for a personalised surgical approach tailored to the patient’s unique anatomy.
- Potentially Improved Outcomes: The use of robotic technology can contribute to improved joint function and longevity of the hip implant.
While robotic-assisted surgery offers many potential benefits, it is important to note that, like any surgical procedure, it is not without risks. Patients should discuss the potential risks and benefits with Dr Tulloch to make an informed decision. Recovery times can vary depending on the individual, but the goal is always to facilitate a safe and effective return to daily activities. Dr Tulloch and his team will provide comprehensive post-operative care and rehabilitation advice to support a smooth recovery process.
Both the use of patient-specific instruments (PSI) and robotic tools highlight Dr. Tulloch’s commitment to excellence in hip replacement surgery. By integrating these advanced technologies, Dr. Tulloch ensures that your treatment plan is meticulously tailored to your unique needs, with the aim of restoring your mobility and enhancing your quality of life.
Hip Replacement Prosthetic Implants: Design, Structure, And Durability
In hip replacement surgery, selecting the appropriate prosthetic implant is crucial as it significantly impacts the success of the procedure, your recovery, and your future mobility. Prosthetic hip implants are sophisticated devices designed to replicate the natural movement of the hip joint. They consist of several key components: the acetabular component (hip socket), the femoral component (thigh bone end), and the articular interface (the surface that enables smooth joint movement).
Each component is engineered for durability, functionality, and biocompatibility, with the goal of restoring hip function and alleviating pain.
FEMORAL COMPONENT
The femoral component is the part of the hip implant that fits into your thigh bone (femur). It is a metal stem inserted into the marrow cavity of the femur and plays a key role in anchoring the artificial joint. This component is designed to integrate with your bone over time, helping to provide long-term stability and support.
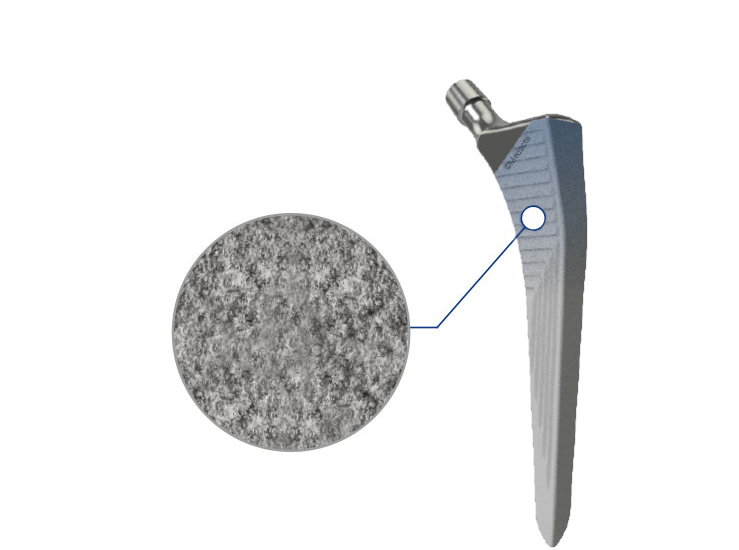
Dr Tulloch selects from a range of femoral components based on each patient’s anatomy, bone quality, and activity level. One commonly used option he uses is the Quadra-P Stem. This is a modern femoral implant engineered to promote both strength and longevity. It features a MectaGrip surface coating, which encourages bone integration by enhancing the connection between the implant and your natural bone. This secure fixation helps improve joint stability and reduce the risk of loosening over time.
Its design supports even load distribution through the femur, which may help reduce stress on surrounding bone. This makes it a suitable choice for patients with active lifestyles or those seeking a durable implant with reliable long-term performance.
Dr. Tulloch will determine the most appropriate femoral component for your hip replacement based on your individual needs and surgical goals.
ACETABULAR COMPONENT
The acetabular component replaces the socket part of your hip joint (the acetabulum). It is a metal cup that fits into the pelvis and forms one half of the new joint, working together with the femoral head to allow smooth, pain-free movement.
This component is designed to securely fix to your bone and hold a liner, typically made of durable plastic or ceramic, which provides a smooth surface for joint movement. The goal is to restore mobility, reduce pain, and replicate the natural function of the hip.
Dr Tulloch commonly uses the M-Pact acetabular cup for total hip replacements. These are a modern, modular acetabular implant designed to achieve stable fixation and promote long-term bone integration. It features a roughened surface that encourages the bone to grow onto the implant, helping to secure it in place without the need for bone cement in most cases.
This design allows for flexibility in choosing the liner type (such as ceramic-on-polyethylene), which can be tailored to suit your age, activity level, and specific joint needs. The M-Pact cup also offers reliable stability, aiming to minimise wear and reduce the risk of dislocation.
Dr. Tulloch will select the most appropriate implant configuration based on your anatomy, bone quality, and lifestyle, with the aim of restoring function and improving long-term outcomes.

ARTICULAR INTERFACE
The articular interface refers to the moving parts of your new hip joint, the femoral head (ball) and the liner inside the acetabular cup (socket). Together, these components create a smooth, gliding surface that allows the hip to move comfortably and efficiently, replicating the function of your natural joint.
The femoral head can be made from ceramic or metal, while the liner is typically made from a type of polyethylene (plastic) or ceramic. The combination of these materials influences how the joint performs over time, including its resistance to wear and risk of dislocation.
Dr. Tulloch frequently recommends a ceramic-on-polyethylene articulation. This pairing involves a ceramic femoral head and a highly cross-linked polyethylene liner, which has been shown to offer excellent durability and low wear rates. This combination is commonly used in both active and older patients and is supported by long-term clinical data.
The selection of your articular interface is based on several factors, including your age, activity level, bone quality, and overall health. Dr Tulloch will guide you through these choices to ensure the components selected align with your individual needs and goals for recovery.

Understanding The Risks Of Hip Replacement Surgery
Hip replacement surgery is a highly effective procedure for alleviating pain and restoring mobility in patients with severe hip joint damage. Like any major surgical procedure however, it comes with certain risks.
Here are the key risks associated with hip replacement surgery:
- Risk of Infection: Although uncommon, infections can occur at the incision site or within the hip joint itself. Such infections may require further treatment, including antibiotics or additional surgery. Dr. Tulloch follows strict sterilisation protocols and provides careful post-operative care to minimise this risk.
- Blood Clots (Thrombosis): Blood clots can form in the veins of the leg (deep vein thrombosis) or, more rarely, travel to the lungs (pulmonary embolism). These conditions can be serious and require immediate attention. Preventative measures, such as blood-thinning medications and compression devices, are used to reduce this risk.
- Implant Loosening or Wear: Over time, the hip implant may wear out or become loose, potentially causing pain and affecting hip function. This is more likely in patients who engage in high-impact activities or have higher body weight. The modern implants used by Dr Tulloch are designed for durability, but revision surgery may be necessary in the future.
- Dislocation: There is a risk of the hip joint dislocating if the ball comes out of the socket, particularly in the early stages of recovery. Dr. Tulloch employs advanced techniques to enhance joint stability and reduce this risk, especially during the critical healing period.
- Nerve or Blood Vessel Damage: During surgery, there is a possibility of injuring the nerves or blood vessels near the hip joint, which can result in numbness, weakness, or circulatory issues. Dr. Tulloch’s precise surgical approach aims to minimise the risk of such complications.
- Leg Length Discrepancy: Some patients may notice a difference in leg length after surgery. Dr. Tulloch takes great care to equalise leg lengths during the procedure, though minor discrepancies can occur. Post-surgical physiotherapy often helps address any resulting issues.
- Allergic Reactions: In rare cases, patients may have allergic reactions to the materials used in the implants. Dr Tulloch conducts thorough assessments to identify any potential allergies and selects the most appropriate materials for each patient.
- General Surgical Risks: As with any surgery, there are risks associated with anaesthesia and the body’s healing process, including adverse reactions to anaesthesia, bleeding, and wound healing complications. Comprehensive pre-operative assessments and vigilant post-operative monitoring are in place to manage these risks.
- Long-Term Risks: Even after a successful hip replacement, there are long-term risks such as implant wear and the potential need for revision surgery. Regular follow-up appointments with Dr. Tulloch help detect and manage any issues early.
Dr. Tulloch is committed to providing the highest standard of care by focusing on reducing these risks through careful patient selection, advanced surgical techniques, and thorough post-operative care.
Benefits Of Hip Replacement Surgery

Hip replacement surgery can significantly enhance your quality of life by addressing severe hip joint damage. Dr Scott Tulloch is committed to developing a personalised care plan that takes into account your specific needs and health goals, aiming to provide you with the best possible outcome.
Potential Benefits of Total Hip Replacement Surgery
- Pain Management: Hip replacement surgery may lead to a reduction in hip pain. By addressing the damaged joint surfaces that contribute to discomfort, the surgery can help you manage pain more effectively.
- Improved Mobility: Many patients report improved hip mobility and range of motion after surgery. Replacing the damaged components of your hip with prosthetics can help you move more comfortably and may make daily activities easier.
- Enhanced Daily Functioning: Following hip replacement surgery, you may find it easier to perform everyday tasks, such as walking or climbing stairs. This improvement in joint function can help increase your independence and ability to engage in various activities.
- Potential for Greater Independence: By improving your hip function, surgery may enable you to perform daily activities with less reliance on others, which can contribute to an improved sense of well-being.
- Longevity of Results: Modern hip implants are designed for durability, with many lasting over 20 years. This means that the benefits of the surgery could potentially be long-lasting, though individual outcomes vary.
- Return to Activities: After sufficient recovery, you may be able to return to low-impact activities like walking, swimming, or cycling. It’s important to discuss your activity goals with Dr. Tulloch to ensure they align with your post-surgical rehabilitation plan.
Pain Management After Total Hip Replacement Surgery
Effective pain management is a vital part of the recovery process following total hip replacement surgery. Dr. Tulloch adopts a comprehensive, multimodal approach to ensure that your discomfort is minimised, allowing you to focus on regaining mobility and returning to your daily activities as smoothly as possible.
Here’s an overview of the pain management strategies that may be utilised:
Pre-Emptive Analgesia: Before surgery, you may receive medications designed to reduce pain and inflammation. This proactive approach can help lessen the intensity of pain immediately following the procedure.
Anaesthesia: During the surgery, a combination of a low-dose spinal anaesthetic, a nerve block, and a light general anaesthetic is often used. This combination effectively manages pain during the procedure and provides extended relief in the immediate postoperative period.
- Medications: A variety of medications may be prescribed to manage pain after surgery, including:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Help reduce inflammation and pain.
Opioids: May be prescribed for short-term use to manage more intense pain.
Acetaminophen: Often used alongside other medications for additional pain relief.
Nerve Pain Medications: Medications like gabapentin or pregabalin may be used to manage nerve-related pain.
- Multimodal Pain Management: Combining different types of pain relief can be more effective than using a single method. This approach targets various pain pathways, providing comprehensive pain control with fewer side effects.
- Nerve Blocks: A nerve block may be administered during surgery to provide extended pain relief. This involves injecting a local anaesthetic near the nerves supplying the hip, helping to numb the area and reduce postoperative pain.
- Ice Therapy: Applying ice packs to the surgical area can help reduce swelling and numb pain. Cold therapy is usually recommended at regular intervals during the initial days after surgery.
- Compression Shorts: Post-operative compression shorts are specifically designed to support recovery after total hip replacement surgery. These shorts fit snugly like bike shorts and feature strategically placed pockets over the surgical incision sites, suitable for all surgical approaches. The pockets are designed to hold ice packs, allowing for targeted cooling therapy to reduce swelling around the surgical site and incorporate compression strips that apply gentle, consistent pressure over the incision areas, which can help reduce swelling and support healing by promoting better circulation.
See here: www.poc-wear.com
- Physiotherapy | Early Mobilisation: Gentle movements and exercises soon after surgery can help manage pain and improve circulation. Physiotherapists will guide you through a personalised exercise plan designed to enhance recovery while minimising discomfort.
Supportive Devices | Walking Aids: Using crutches or a walker initially can help reduce pressure on the new hip joint, alleviating pain as you begin to move around.
Follow-Up Appointments: Regular follow-ups with Dr. Tulloch are essential to monitor your pain levels and adjust your pain management plan as needed, ensuring that your recovery progresses smoothly
By implementing a comprehensive and individualised pain management plan, Dr. Tulloch aims to ensure your comfort and support a faster, smoother recovery following total hip replacement surgery. The goal is to minimise pain, enhance your mobility, and help you return to your normal activities as quickly and safely as possible.
Recovery Following Total Hip Replacement Surgery
The recovery phase after total hip replacement is the beginning of your journey toward regaining mobility and improving your quality of life.
IMMEDIATELY AFTER SURGERY
You will wake up in the Recovery Unit, although you may not remember this part. An X-ray will be taken to confirm everything looks as expected. Nurses will monitor you closely to ensure you have recovered well from the anaesthetic, and any IV tubes will likely be removed at this time.
- Returning to the Surgical Ward: Once these steps are complete, you’ll be moved to the surgical ward. Here, you’ll be encouraged to eat and drink to regain energy. Hydration is important, so try to drink at least 2 or 3 glasses of water.
- Preventing Blood Clots: Your legs will be fitted with compression stockings, and you may also have foot pumps, which are Velcro devices that gently squeeze your feet to encourage blood flow and prevent clots.
- Surgical Site and Pain Management: Your leg will be bandaged, and you’ll have a small anaesthetic infusion device near your hip, resembling a ball. The surgical area may appear pink from the preparation process. You’ll also be given medication to manage pain effectively, allowing you to start moving as soon as possible.
- Getting Dressed: After eating and drinking, you should get dressed in loose, comfortable clothes. If you need assistance, the nursing staff will be there to help.
PAIN MANAGEMENT
Managing your pain is a priority immediately after surgery. You’ll receive medications tailored to control your pain levels, enabling you to start moving and walking soon after the operation. It’s crucial to inform the hospital team if your pain isn’t well controlled. Pain relief, combined with swelling management techniques such as rest, ice, elevation, and compression, plays a significant role in your recovery.
MONITORING AND WOUND CARE
Your healthcare team will closely observe your recovery, paying special attention to your wound to ensure its healing properly and showing no signs of infection.
REHABILITATION AND PHYSIOTHERAPY
From day one, you’ll begin a rehabilitation program designed to strengthen your hip muscles and improve mobility. Within 4 hours of surgery, you’ll be encouraged to get out of bed and walk. A nurse or physiotherapist will supervise your first steps, and you’ll use a walking aid such as a frame, crutches, or a stick. You will be allowed to put full weight on your leg from the start.
HOSPITAL STAY
Most patients stay in the hospital for 48 to 72 hours, depending on the complexity of the surgery, your overall health, and recovery progress. In some cases, you may even be able to go home the same day.
1-2 WEEKS POST-OP
- Swelling: It’s common to experience swelling from your thigh down to your foot, which may increase during the first few days post-surgery. Elevating your leg and walking can help reduce this swelling, which may persist for up to 12 months but will gradually decrease.
- Bruising and Blistering: Bruising is normal and often appears dramatic due to blood-thinning medications. Blisters may also form near the incision site but typically resolve on their own. Bandages will be changed after about a week, once the wound is sufficiently healed to reduce the risk of infection.
- Muscle Soreness and Heat: You may experience stiffness and soreness in the muscles around the surgical site due to the surgery. This discomfort will gradually improve with walking, stretching, and physiotherapy. The operated area may also feel warm, a sensation that can last up to 12 months as part of the healing process.
- Modified Activity Level: For the first two weeks, your activity will be limited, but you’ll be able to walk independently and perform normal daily activities. The extent of these limitations and your recovery pace can vary depending on the surgical technique used. For example, patients who undergo the anterior approach may experience a quicker recovery and fewer restrictions compared to those who have the posterior or lateral approaches. This is because the anterior approach typically spares more muscle and tissue, allowing for a faster return to mobility. Dr. Tulloch will provide guidance tailored to your specific situation, ensuring that your recovery plan aligns with the surgical technique used.
FULL RECOVERY
- 6 Weeks Post-Op: By approximately six weeks, you can expect to resume most of your normal activities. Full surgical healing typically takes 6 to 8 weeks, during which some swelling and discomfort are normal. Maintaining a positive outlook is essential, as the goal of hip replacement surgery is to relieve pain and stiffness, allowing you to return to the activities you enjoy.
KEY POINTS TO REMEMBER
- Walking: Start with a walking aid and gradually reduce its use as advised by your physiotherapist.
- Driving: You may be able to resume driving around four weeks post-surgery, beginning with short, safe trips.
- Swimming and Hydrotherapy: These activities can usually begin three weeks after surgery, with appropriate wound protection.
- Sports: A gradual return to activities like golf, tennis, and skiing is recommended after 6 to 12 weeks. Avoid contact sports to prevent injury.
- Travel: Short flights may be possible after 5 to 7 days. For longer flights, wait at least six weeks and take precautions against deep vein thrombosis (DVT).
- Airport Security and MRI Scans: Your implant may trigger security alarms but is MRI-compatible, so future imaging tests should not be a concern.
Dr. Scott Tulloch’s approach to recovery is designed to support a smooth transition back to your normal life, with a focus on reducing pain, enhancing mobility, and helping you return to the activities you love.
Post-operative Precautions Following Total Hip Replacement Surgery
After hip surgery, it’s essential to follow specific precautions to ensure proper healing and avoid complications.
ANTERIOR APPROACH Total Hip Replacement Precautions Post-Op:
- Limit hip extension for six weeks following the surgery.
- Do not cross your legs for 6 weeks following the surgery
POSTERIOR APPROACH Total Hip Replacement Precautions Post-Op:
- Avoid Twisting Movements: Keep your hips aligned and avoid twisting at the waist to maintain the stability of your new hip joint.
- Limit Bending: When bending forward, do not go beyond 90 degrees at the hip. This precaution helps prevent dislocation.
- No Crossing Legs: Avoid crossing your legs or ankles, as this can put undue pressure on your hip and disrupt the healing process.
Navigating Insurance And Costs For Total Hip Replacement Surgery
Navigating the financial landscape of health insurance and the costs associated with total hip replacement surgery in Australia requires a clear understanding to ensure you are well-prepared for any expenses. Dr Scott Tulloch provides this comprehensive guide to help you make informed decisions regarding your hip replacement surgery and its financial implications.
Public vs. Private Healthcare Options in Australia
Through Medicare, the Australian government offers coverage for hip replacement surgery at public hospitals, which typically results in minimal direct costs to the patient. However, patients may face extended waiting times and have limited choices regarding their surgeon and the timing of the surgery.
Private health insurance allows access to private hospitals, the choice of surgeon, and typically shorter waiting times. This option is ideal for those who prefer more control over their healthcare decisions and timelines.
Understanding Health Insurance Coverage
Policies vary widely, so it’s crucial to review your coverage in detail. Key aspects typically covered include hospital accommodation, fees for the surgeon and anaesthetist, the prosthetic device, and post-operative rehabilitation.
Be aware of any waiting periods that may apply to pre-existing conditions or specific procedures such as hip replacement surgery. Verifying your coverage details in advance can help avoid unexpected financial surprises.
Health Insurance Tiers and Coverage
Australian private health insurance is categorised into four tiers: Basic, Bronze, Silver, and Gold, with each tier offering different levels of coverage.
For comprehensive procedures like hip replacement surgery, you will typically need a policy in the silver or gold tiers.
- Silver Plans: These plans may cover joint reconstructions and some rehabilitation services. It is essential however to verify whether joint replacements are included, as coverage can vary.
- Gold Plans: These offer the most extensive coverage, including hip replacement surgery and associated rehabilitation services. Gold plans are ideal for those seeking full coverage for complex procedures.
Navigating Medicare and Insurance
Medicare provides rebates for hospital treatment and a portion of the surgeon’s and anaesthetist’s fees for hip replacement surgery. Understanding the specific Medicare item numbers (e.g., 49318 for total hip replacement) is important for knowing what is covered and any potential out-of-pocket costs.
- Out-of-Pocket Expenses: Despite insurance coverage, patients may still incur out-of-pocket expenses for costs not fully covered by Medicare or private insurance, such as extended hospital stays or specific surgeon fees. It’s important to discuss these details with Dr Tulloch and review your insurance policy to anticipate any additional costs.
Pre-Approval and Planning
Obtaining pre-approval from your health insurance provider before undergoing hip replacement surgery is essential to confirm coverage and avoid unexpected costs. This process involves verifying that the specific Medicare item numbers related to your procedure are included in your policy.
Understanding the specifics of your health insurance coverage, including your plan’s tier and the Medicare item numbers it covers, is crucial for effectively managing the costs associated with hip replacement surgery. By staying informed and taking these steps, you can navigate the financial aspects of your hip replacement surgery with confidence, ensuring a smoother and more predictable recovery process.
Self-funding Your Total Hip Replacement: A Guide For Patients Without Private Health Insurance
Opting to self-fund your hip replacement surgery in a private hospital with Dr. Scott Tulloch offers a viable alternative for patients without private health insurance. This option provides timely access to medical care, allowing you to bypass the long wait times often associated with the public healthcare system.
- A Closer Look at Costs: Choosing to self-fund your hip replacement surgery with Dr. Tulloch ensures access to high-quality surgical expertise. The overall cost typically ranges from $24,000 to $30,000, depending on various factors, including the length of your hospital stay and any pre-existing health conditions that may influence the surgery and recovery process.
- Included in that cost estimate are the following components:
- Hospital Accommodation: the cost of your stay in a comfortable environment immediately following your surgery.
- Medical Fees: Includes fees for Dr Tulloch, the anaesthetist, and any assisting surgical staff.
- Prosthesis Costs: Involves the cost of state-of-the-art components, reflecting the high standards that Dr. Tulloch consistently employs.
- Theatre Fee: Covers the use of the surgical facilities during your operation.
- Consultation Fees: Includes two post-operative consultations at Dr Tulloch’s practice to ensure that your recovery is progressing as expected.
Most patients are discharged the day after surgery, which can help reduce overall costs by minimising the need for extended hospital accommodation—typically priced at around $900 per additional night.
Be mindful of potential extra expenses, including pre-operative consultations with Dr. Tulloch, diagnostic imaging, walking aids, compression shorts and follow-up physiotherapy sessions after discharge.
